Dr. Nadja Albertsen is the ESA-sponsored medical doctor spending 12 months at Concordia research station in Antarctica. She facilitates a number of experiments on the effects of isolation, light deprivation, and extreme temperatures on the human body and mind. This blog entry is translated from her original in Danish and was split into two, part one is available here.
After a while you can get to know colleagues, family and friends by the sound of their steps. Some trample, some drag their feet, some limp, some walk fast and others slow. Some walk with heels, others with sneakers and some go bare feet.
This also applies in Concordia. When you spend all your time with the same 12 people, you no longer doubt who is awake for a pee every night at 02:00, or who lists around the floor early in the morning.
Concordia teaches people to recognise another type of sound – breathing. It is not as intimate as it may sound. The base consists of two towers and unless you sneak into the goods elevator, you have to take the stairs up and down many times during the day. On days when taking blood tests for the EFIA project, which I want to write about today, my watch often records 60 floors (up) and I have never recorded less than 25 floors in a day. So when I have trouble finding something positive about a year’s stay in Concordia, hopefully I can boast a firmer back when I return!
But that was a leap from one end of the body to another – back to breathing! Most people breathe as they work their way up the stairs, so often you can hear them before you can see them – and strangely enough, everyone sounds different and some significantly worse (or better if you want to) than others.
Even taking into account fitness, weight and age, the main cause of the every breath in Concordia is the low air pressure – better known as thin air. Concordia is located at an altitude of 3233 meters on the Antarctic plateau, which is approximately the same altitude as the Dolomites – or the same altitude as Tibet’s capital, Lhasa. That means the air is relatively thin here, just like in the mountains, as gravity pulls the air, just like everything else, to the ground.
Now a bit about air and oxygen pressure
This means that air has weight. Due to its weight, air exerts a pressure on the surface below it and this pressure is described as the air pressure. The higher you are, the less air there is above the ground to exert this pressure and the lower the air pressure is. You could also say that there is a longer distance between the constituents air is made of, the different gases, even though their distribution is the same. Thus, at low air pressure, the air will still consist of, among other things, 21% oxygen and the pressure exerted by the oxygen itself – the oxygen pressure – will thus decrease to the corresponding air pressure.
And so that it doesn’t get too simple, more factors influence air pressure than “just” the altitude. Temperature and location for example. The closer you get to the poles, whether north or south, air pressure decreases – because the rotation of the Earth and centrifugal force make the atmosphere thinner the farther away from the equator you move. And the thinner the atmosphere – the less air. The end result is that at Concordia we have an average air pressure equivalent to approximately 3800 m at the equator.
As we know from the weather forecasts, the air pressure fluctuates from day to day – as it does in Concordia too. In fact, we can often judge from the sound level of certain people in the base whether the pressure of a given day is higher or lower than normal. And it is actually incredible how much even small fluctuations can be felt!
The type of oxygen deficiency experience here is called “hypobaric hypoxia” which means oxygen deficiency due to low air pressure. Many comment before leaving Concordia that what they are most looking forward to is to be able to breathe “normally”.
EFIA project
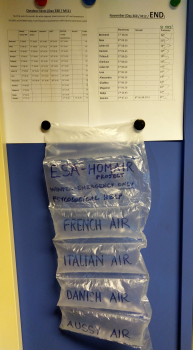
One of ESA’s projects, EFIA, deals mainly with the thin air and the relative lack of oxygen in the base. EFIA stands for Edema Formation in Antarctica (= edema formation / fluid accumulation in Antarctica) and it from a German team who have done similar studies in the thin mountain air and on fluid distribution in people who are placed in bed with their head tilted slightly down, mimicking the effect of weightlessness in the room.
The EFIA project focuses on how we respond to the thin air. Most of us arrive at Concordia in the beginning of the Antarctic summer and move from sea level to 3200 m above in just a few hours –giving the body a shock by the sudden lack of oxygen. We risk developing altitude sickness upon arrival, and most experience symptoms to a greater or lesser extent, while the severe forms of acute mountain sickness fortunately are rare on base – it has happened that someone has been so sick that they had to fly back to the coast – but doesn’t happen every year thankfully.
The EFIA project studies the reactions that occur in the body immediately after arrival, how they react over time and how we, the subjects, feel. Hopefully this study will help understand who develops symptoms of altitude sickness and who does not and why – we do not know very much about it. We know that if you have had it once, you are at greater risk of getting altitude sickness than those who have not had it before. Increased knowledge could, among other things, open up the possibility of both preventing and treating altitude sickness in connection with mountain (and Antarctic) living, but also find out if anyone is better suited to stay in thin air than others – and if so, who. And it’s actually really interesting in relation to space travel!
Space pressure
 As you know, there are many similarities between Concordia and traveling in space including that we have to bring all supplies “from home” with the exception that we have water and air here – two things take much space and weight in spacecraft. And when something weighs a lot and takes up a lot of space, it takes fuel to move – so a really exciting aspect of the EFIA project is whether you can assess how little oxygen humans can settle with while still functioning normally. The less oxygen, the less weight, and the less fuel you need to spend (and bring) on trips into space (or you can bring other things, such as liquorice pipes and bacon wraps).
As you know, there are many similarities between Concordia and traveling in space including that we have to bring all supplies “from home” with the exception that we have water and air here – two things take much space and weight in spacecraft. And when something weighs a lot and takes up a lot of space, it takes fuel to move – so a really exciting aspect of the EFIA project is whether you can assess how little oxygen humans can settle with while still functioning normally. The less oxygen, the less weight, and the less fuel you need to spend (and bring) on trips into space (or you can bring other things, such as liquorice pipes and bacon wraps).
To study the immediate effect of the thin air, I assaulted the team as the plane had put the skis down on the ice. I arrived in Concordia a few weeks before the rest of the group, and was ready with blood pressure cuffs, questionnaires and blood test equipment almost as they entered the door. They were tested on day 2, day 7, day 14 and 31 – and then every month for the first six months. Now they are only hunted every two months.
The “easy” part of the study is two questionnaires on symptoms of altitude sickness. These are the same charts used by mountaineers who examine how people feel – not what you can measure or weigh, but subjective feelings. The questions cover headaches, nausea, insomnia, appetite and dizziness and rate severity on a scale from 1 to 4. Often the symptoms will be worse in the morning and fade during the day when you’ve been active and oxygen is pumped around the body – that’s why we have to fill the forms in the morning and evening. The nice thing about the questionnaires is that they are quick to complete and it is something people can do on their own. On the other hand, questionnaires presume that people are able to answer the questions honestly and so must be interpreted with some caution if you want to compare between different people – a headache that scores a 2 for one person, might score a 0 or 4 in another. But questionnaires are excellent at following changes of the same person!
The questionnaires will of course also be compared with, among other things, the blood test responses when the many tubes return to Germany and are analysed in 2020. It will be interesting (and important) to see if the symptoms experienced have a direct correlation between changes in blood or not.
In addition, weight, blood pressure, heart rate, oxygen saturation in the blood and the amount of carbon monoxide (CO) in the exhaled air is recorded for each subject.





Discussion: one comment
I WOULD FIND IT DIFFICULT TO BE IN ANY LOCATION WHERE I MUST THINK ABOUT HOW TO BREATH!
JOHN LINZINMEIR